
Toxic shock syndrome (TSS) is a rare and often life-threatening illness that develops suddenly after a bacterial infection. It can affect different organ systems, including the kidneys, lungs, and liver causing multiple organ failure. TSS progresses quickly; therefore, immediate medical treatment is needed.
Causes
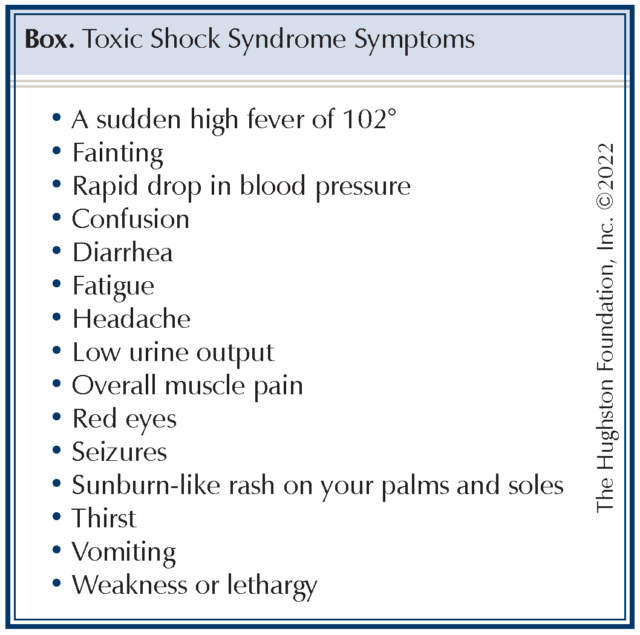
TSS is caused by the body’s sudden and massive immune response to toxin-producing strains of gram-positive bacteria—Staphylococcus aureus and Streptococcus pyogenes (group A streptococcus). These toxins that act as superantigens over stimulate a normal immune-cell response and overwhelm the body’s normal functions. A patient’s symptoms can mimic other illnesses, but with TSS, these symptoms can worsen rapidly (Box). Symptoms often include a high fever, vomiting, diarrhea, a sunburn-like rash, and signs include low blood pressure and shock including confusion, dizziness, or fainting. During orthopaedic surgery, the acute onset of TSS is rare; however, due to the serious nature of this disease, it is important for surgeons to recognize it to begin immediate treatment.
Risk factors
TSS can affect men, children, and women of all ages; however, about half of all patients with staphylococci bacteria occur in women of menstruating age. Risk factors for TSS include skin wounds, surgery, and the use of tampons and other devices, such as menstrual cups, contraceptive sponges, or diaphragms. Additionally, TSS is associated with infections, for example cellulitis (bacterial skin infection), pneumonia (viral or bacterial lung infection), or osteomyelitis (bacterial bone infection). It is also important to note that if you have had TSS before, you should discuss this with your physician or surgeon before you receive any medical treatment. People who have had TSS before are at a higher risk of it getting it again.
Osteomyelitis and TSS
In orthopaedics, long bone infections and chronic osteomyelitis are common diagnoses. The number of bony infections relates to the prevalence and severity of injuries, particularly due to motor-vehicle accidents. The treatment of open extremity injuries or established infections in long bone fractures usually involves a prolonged course of antibiotics, wound debridement (removal of damaged tissue), and fracture stabilization.
TSS has been associated with a variety of surgical procedures and with postoperative abscesses. The source of infection is commonly acquired at or near the time of surgery and has been described following nasal packing, insertion of hardware, surgical drains, and retained foreign materials.
Diagnosis
There is no single test for TSS and doctors often diagnose it in an emergency setting. Your doctor will order blood and urine samples to test for the presence of a staph or strep infection. For a female patient, the doctor may also order swab testing of the vagina, cervix, and throat for the presence of the bacteria. Since TSS can affect your organs, the doctor may order a CT scan, a lumbar puncture to test spinal fluid for bacteria, or a chest x-ray to assess the extent of your illness.
Treatment
Patients with TSS are often hospitalized, sometimes in the intensive care unit, and treated with antibiotics, while doctors seek the source of the infection. While in the hospital, you will receive care for your other symptoms, such as stabilizing your blood pressure, reducing your fever, and pain medicine for muscle aches and headaches. Additionally, the toxins produced by the bacteria and accompanying hypotension can cause kidney failure. If that happens, you may need dialysis.
A medical emergency
Call your doctor or surgeon immediately if you experience any symptoms of TSS, especially if you have recently had surgery or a skin or wound infection. TSS is a medical emergency that cannot be treated at home. It can progress rapidly, causing serious complications such as shock and renal (kidney) failure, and even death.
Author: Christopher R. Rehak, BS, and Michael Ulmer, DO | Columbus, Georgia
Last edited on December 22, 2022