Contributing physicians in this story


Lumbar (low back) pain is widespread with up to 84% of individuals experiencing back pain within their lifetime.¹ Physicians define chronic lumbar pain as back discomfort lasting longer than 12 weeks. There are many causes of low back pain—lumbar strain, degenerative disc disease (Fig. 1A), lumbar stenosis, inflammatory autoimmune diseases—all of which require a specific treatment approach. There are 3 types of low back pain: 1) referred pain, which feels dull and achy and sometimes moves around and varies in intensity; 2) axial pain, which can range from sharp, shooting pain to dull and achy while remaining in one specific spot or region; and, 3) radicular pain, is excruciating, burning, or stinging pain caused by compression or inflammation of a spinal nerve root. Sometimes there is no definitive finding to explain the discomfort. In any case, an orthopaedic spine specialist can give you an appropriate physical exam to properly diagnose the problem and tailor a specific treatment.
Diagnosing low back pain
The diagnosis of chronic low back pain begins with a formal examination by a health care provider, and can include x-rays as well as a neurologic examination. Characterization of the discomfort is important. People may experience numbness and/or tingling, leg pain (one leg or both) which may include cramping. Neurologic examination, including deep tendon reflexes, motor strength, and sensory findings, can help localize the exact lumbar level. Neurologic symptoms including weakness, fevers, and leg pain may warrant a magnetic resonance imaging (MRI) or computed tomography (CT) scan (tests that shows bones, muscles, tendons, and ligaments) to better diagnose the exact etiology, or causes.
Nonsurgical treatment
Nonpharmacological treatments include home-based therapy exercises, formal physical therapy, and manual manipulation. Your doctor may use a combination of these approaches and tailor them to your specific needs. Therapy can be particularly important with focus on isometric core strengthening exercises (muscle contraction without joint movement) and stretching targeted tight muscle groups. Aerobic exercises have been shown to improve pain, disability, and mental health in patients who have chronic nonspecific axial low back pain.² Exercises such as yoga, Pilates, and tai chi can be helpful as well. Physicians often prescribe aquatic therapy to older patients since it offers low stress on the joints. Specific modalities, such as dry needling, can be used and has been seen to help patients who have chronic low back pain.³ Cognitive behavioral therapy combined with a well-balanced therapy program can be a useful adjunct to further decrease back pain.
Pharmacologic treatment options can supplement a therapy program. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen are first-line drugs. The success of this treatment solely depends on the patient’s ability to tolerate the medication. NSAIDs can cause gastrointestinal issues and may negatively affect kidney function. When a patient cannot tolerate NSAIDs, their physician may recommend acetaminophen or weak opiates.
Topical medication options can be useful as a short-term treatment. Lidocaine patches, topical NSAIDs, or topical menthol are just a few of the topical medications that can be used. Physicians do not recommend long-term narcotic use for low back pain. Narcotics can result in dependence and even increase pain. Opioid induced hyperalgesia, a phenomenon doctors see with chronic narcotic use, results in increased sensitivity to painful stimuli and magnifies the pain response.
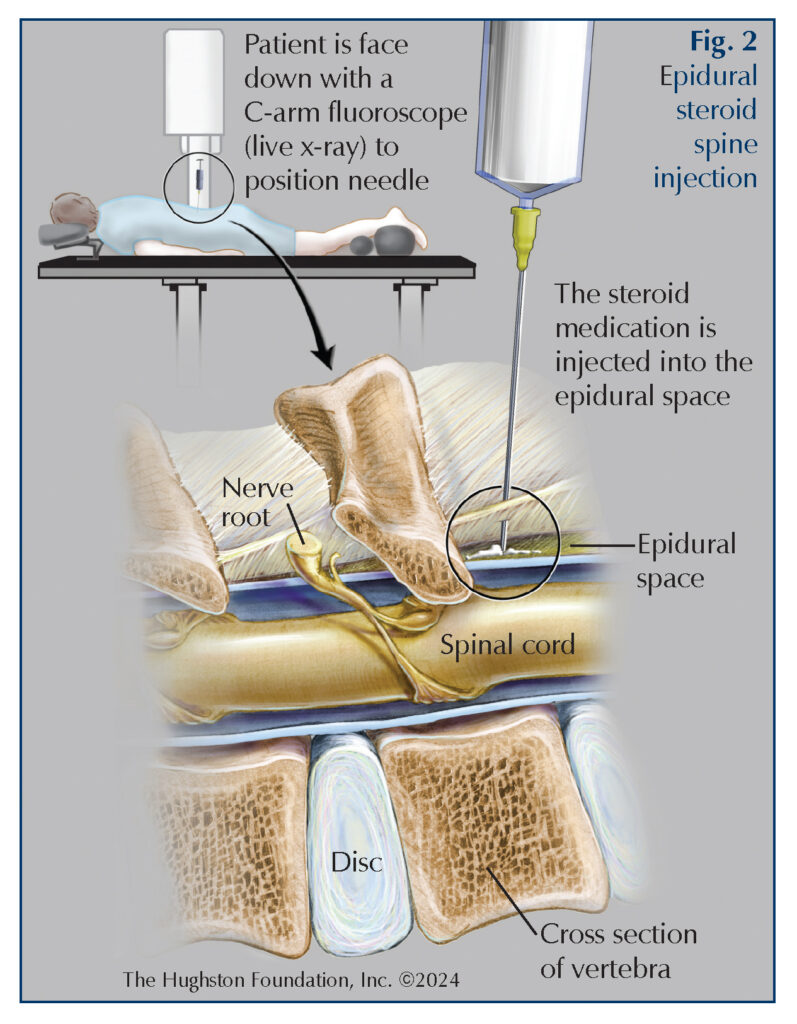
Injections and radiofrequency ablation treatments can help control pain. Injections can vary from epidural steroid injection (Fig. 2), selective nerve root blocks, medial branch blocks, facet injections, and radiofrequency ablation. Physicians, surgeons, radiologists, and pain management specialists can administer these treatments.
For patients who are not good surgical candidates, spinal cord stimulators (implant that sends low-level electricity into the spinal cord) can be an alternative. Physicians often use a temporary trial device to see if spinal cord stimulation could be an effective treatment option. For patients who continue to have significantly limiting pain, despite using multi-modality treatments, their physician can refer them to a pain management specialist.
Surgical treatment
Doctors reserve surgery for patients who have specific pathology, including severe stenosis (compressed spinal cord) or marked instability resulting in significant functional disability. Surgical options include fusion (bones fused together permanently), disc arthroplasty (replace disc with implant) (Fig. 1B), or laminectomy (decompression surgery). Without neurologic decline/deficit, there should be a complete failure with multi-modality conservative management before proceeding with surgery. Surgery in the setting of chronic back pain has the potential for causing worse pain and thus spine surgeons do not make a recommendation lightly.
Managing the pain
Identifying the cause of chronic back pain can be extremely difficult. There are multiple treatment options—therapy and its related modalities, pharmacologic treatment options including both narcotic and non-narcotic, and lastly, surgery. Ultimately, the treatment success lies with the patient’s understanding and expectations, especially since treating chronic back pain is often not about achieving complete pain relief, but rather, managing the pain effectively and improving overall quality of life.
Author: Gil Gomez, DO | Columbus, Georgia
References:
- Airaksinen O, Brox JI, Cedraschi C. et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur. Spine J. 2006;15(Suppl 2):S192-S300.
- Kreiner DS, Matz P, Bono CM, et al. Guideline summary review: An evidence-based clinical guideline for the diagnosis and treatment of low back pain. Spine J. 2020;20:998-1024.
- Rajfur J, Rajfur K, Kosowski L, et al. The effectiveness of dry needling in patients with chronic low back pain: a prospective, randomized, single-blinded study. Sci Rep. 2022;12(1):15803.
Last edited on July 2, 2024