
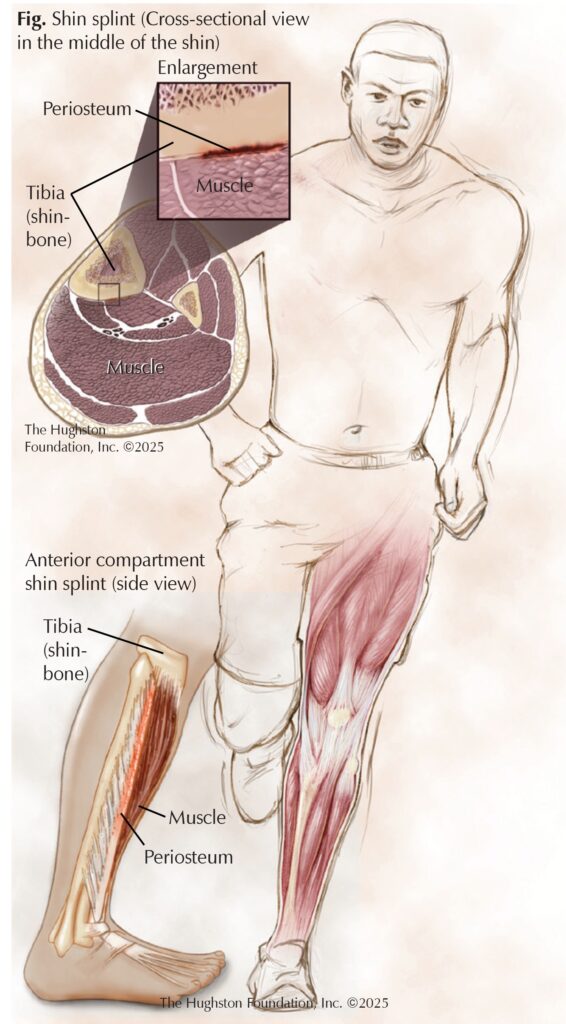
Medial tibial stress syndrome (MTSS), commonly referred to as shin splints, affects up to 35% of athletes each year. Shin splints involve pain along the anteromedial (front-inside) of the tibia, or shinbone (larger bone of the lower leg) (Fig). The first known mention of shin splints occurred in 1958; however, it suffices to say that people suffered from the condition long before. Of note, a recent archeological team uncovered a 500- to 800-year-old skeleton with features consistent with MTSS.
Symptoms
MTTS often occurs bilaterally, meaning in both legs, and felt at the middle to distal (closer to ankle) portion of the lower leg. Pain often arises during the beginning and at the end of workouts and tends to subside around the mid-point of an activity. The pain often disappears with rest but may persist for a short time, depending on the chronicity of the condition. If MTSS has become chronic, the pain may last longer into exercise, persist even after cooling down, and become almost constant. MTSS is a gradual-progressive condition, often exacerbated as the athlete continues training, leading to worsening symptoms with each activity.
Risk factors
MTSS tends to occur in athletes exerting forceful energy against the ground, which explains why it often affects runners, jumpers, and new military recruits. However, it also results from overuse of the lower extremities. The true culprit comes from a sudden change in volume or intensity of training, which particularly appears in runners increasing their activity and new military recruits who suddenly begin long runs or daily marches. A classic case can happen when a patient who runs 1 to 2 miles a day decides to start training for a marathon, running 9 to 10 miles per day, and develops anteromedial lower leg pain. Other common causes include footwear with minimal cushion, running on uneven or hard surfaces, improper warmup, and foot abnormalities in conjunction with increased running volume.
Among the foot abnormalities are flat feet and hyperpronation (inward rolling). Hyperpronation causes improper biomechanics of the lower extremity, creating undue stress on the tibia and muscles of the lower leg. These features combined create microfractures of the bone and traction periostitis (inflammation of the covering of bones) due to either the soleus, flexor digitorum longus, or tibialis posterior pulling on the bone to perform lower extremity movements. The periostitis and microfractures involve cytokine (chemical messengers) release, which promotes pain, swelling, and tenderness. The condition is more common in women, those with higher body mass indexes (BMI, a measurement often used to determine healthy weight status), smokers, and people with vitamin D deficiency.
Medical evaluation
Often, people who suffer from shin splints do not undergo a formal medical evaluation. The symptoms are often self-limiting to the point that people decrease their activity to reduce the pain, which results in symptoms either improving or diminishing. When a patient does see a doctor, MTSS is diagnosed by history and physical examination alone. On physical examination, there may be pain on percussion (tapping) of the shinbone or tenderness to palpation (pressure) in the symptomatic area. During physical examination, the patient walks and demonstrates range of motion of the ankles, knees, and hips. The physician can also provide resistance to plantarflexion (pointing toes toward the ground), which will provoke pain. Imaging, including computed topography (CT or CAT scan) and magnetic resonance imaging (MRI) are rarely needed unless you have swelling, redness, or loss of sensation.
Treatment
Conservative therapies include rest, activity modification (such as swimming instead of running), icing, stretching, and wearing compression stockings. Resting is the most popular treatment as it combats the overuse that causes MTSS. In the acute phase (first onset), resting, icing, and nonsteroidal anti-inflammatory drugs, such as ibuprofen or naproxen sodium are more beneficial, but as time progresses, activity modification helps to mitigate future symptom flare-ups. Recovery should be gradual since setbacks can occur. If you start exercising again and the pain recurs, take a few days to rest. Then, you can start at a less intense activity level and increase the intensity more gradually than before, giving your body time to adapt to the new stresses. Rarely do you need surgery for shin splints.
Avoiding Chronic MTSS
Most people can adapt to MTSS with few issues by listening to your body and finding what works best for you. However, returning right back to previous activity levels without modification or intensity changes can cause a recurrence of symptoms. You should adjust your routine upon onset, since avoiding recovery can prolong your symptoms and lead to the development of chronic MTSS, where pain persists even after exercise, or leads to a stress fracture. Chronic MTSS can be difficult to overcome, so pushing through the pain is not wise.
Prevention
You can avoid shin splints altogether by taking a few preventive measures. First, make sure your shoes are designed for your sport. For example, runners should wear running shoes and basketball and tennis players should wear court sneakers. You should also cross train to take a day off from your usual regimen. You can substitute a jogging day with a lower impact exercise such as cycling. Take it slow, increase your time or distance gradually, so your body can adjust to the change.
Authors: Austin Helton, BS, and Nicholas Cavil, MD | Columbus, Georgia
Last edited on July 15, 2025