
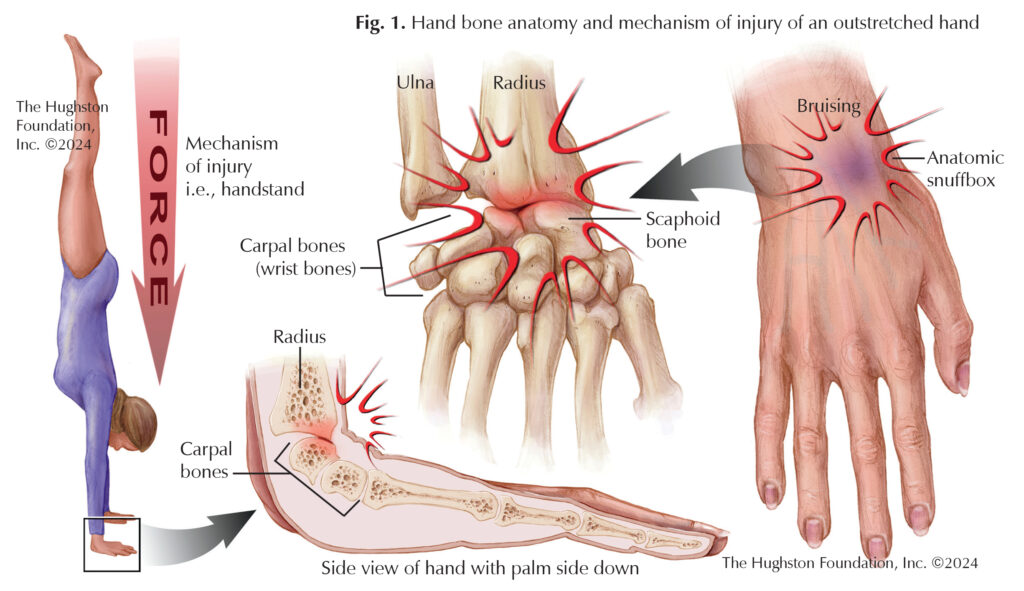
The carpus, or wrist, contains 4 bones in 2 rows for a total of 8 bones. The scaphoid is a boat shaped bone in the wrist and is the keystone for the other bones. In architecture, the keystone is a central stone at the top of an arch that links and locks the structure together (Fig. 1). The scaphoid acts as the keystone for the carpal bones and links the 2 rows together. It is also the most commonly fractured carpal bone in the wrist.¹ Younger patients often injure the bone during sporting events while older patients tend to fracture the bone during a fall on an outstretched hand.
Symptoms
A patient who has a scaphoid injury often presents with pain and swelling on the radial (thumb) side of the wrist. Occasionally, bruising may be present. The injury can also present as pain at the anatomic snuffbox (base of the thumb). The patient often has limited motion of the wrist, especially while pushing on an object with the wrist extended (backwards). If you have an injury along with any of the above signs or symptoms, especially if they persist more than a few days, then you should have your hand and wrist evaluated by an orthopaedist.
Screening and diagnosing your injury
During your clinic evaluation, your physician will ask you about the history of your injury and examine your wrist, checking for tenderness, and range of motion. Your doctor can order radiographs (x-rays) of the wrist to determine if you have a fracture. Due to the nature of a scaphoid fracture, it may not appear on radiographs for up to 2 weeks after injury. If this is the case, options are available. Your physician may have you return to clinic for repeat radiographs. Alternatively, if there is a high suspicion, your physician can elect to complete a magnetic resonance imaging (MRI) of the wrist to evaluate for an occult (hidden) fracture.²
Types of scaphoid fractures and treatment
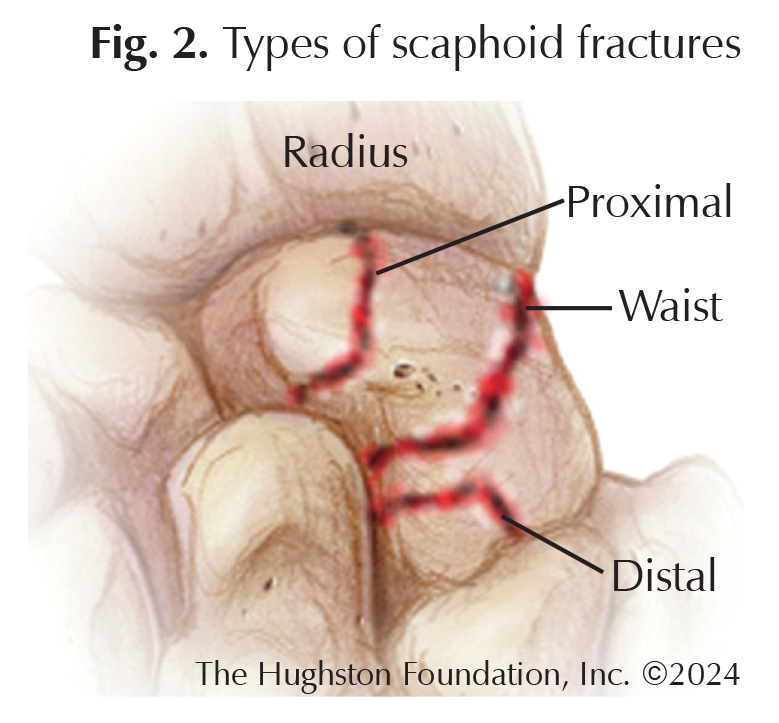 The scaphoid is divided into 3 parts: proximal pole, waist, and distal pole (Fig. 2). The presence of blood flow to the scaphoid drives the treatment plan. Blood enters the scaphoid at the distal pole and then has retrograde (reverse) flow to the proximal pole. Based on imaging, your orthopaedist can determine the location of the scaphoid fracture and displacement (how far apart the fracture fragments are). Using this information, your doctor will develop an appropriate treatment plan tailored to you and your injury.
The scaphoid is divided into 3 parts: proximal pole, waist, and distal pole (Fig. 2). The presence of blood flow to the scaphoid drives the treatment plan. Blood enters the scaphoid at the distal pole and then has retrograde (reverse) flow to the proximal pole. Based on imaging, your orthopaedist can determine the location of the scaphoid fracture and displacement (how far apart the fracture fragments are). Using this information, your doctor will develop an appropriate treatment plan tailored to you and your injury.
Distal pole
Since the distal pole has a good blood supply, doctors often treat a fracture with a cast for 4 to 6 weeks. The specific type of cast is determined by the orthopaedist but a variety of casts can be used for successful union (healed fracture).³ If the fracture has significant displacement (>1.5 mm), then operative treatment is preferred.²
Waist
Physicians treat scaphoid waist fractures either operatively or nonoperatively. After cast treatment, union occurs for approximately 90% of non- or minimally-displaced scaphoid waist fractures. Operative treatment can also be considered as it has the advantage of earlier return to function by 3 weeks.² Operative treatment is definitively indicated if the fracture is displaced more than 1.5 mm.
Proximal pole
The proximal pole of the scaphoid has a tenuous (weak) blood supply, an articular surface (joint) on one portion, and ligamentous attachment (tissues connecting bone) on the other. For these reasons, proximal pole fractures are often treated operatively.¹
Complications
The most common complications of scaphoid fractures are delayed union, nonunion, arthritis, reduced wrist motion, and loss of strength. If untreated or undiagnosed, it can lead to a degenerative condition known as scaphoid nonunion advanced collapse (SNAC wrist), which eventually causes abnormal joint movement, reduced grip and pinch strength, stiffness, and pain.
Follow-up care
Depending on the fracture, your doctor can treat the injury with cast immobilization or surgery. Typically, you will follow-up with your orthopaedist 2 to 4 weeks post-injury. At the clinic visit, the doctor may remove the cast or splint to examine the skin, and take new radiographs to see how the fracture is healing. Most fractures will heal with immobilization, but depending on the fracture location, it can take 3 months or more to heal.
Author: Darren Patel, DO | Columbus, Georgia
References:
- Wolfe SW, Pederson WC, Kozin SH, Cohen MS. Green’s Operative Hand Surgery. 2-Vol, 8th Ed. Cambridge, MA: Elsevier; 2021.
- Clementson M, Bjorkman A, Thomsen NOB. Acute scaphoid fractures: guidelines for diagnosis and treatment.” EFORT Open Rev. 2020;5(2):96-103.
- Buijze GA, Gosling JC, Rhemrev SJ, et al. Cast immobilization with and without immobilization of the thumb for nondisplaced and minimally displaced scaphoid waist fractures: a multicenter, randomized, controlled trial. Journal of Hand Surgery. 2014;39(4):621-7
Last edited on September 13, 2024