According to the Centers for Disease Control and Prevention (CDC), traumatic injuries are the leading cause of death for American children and adults ages 1 to 44. The CDC reports that the leading causes of trauma are motor vehicle accidents, falls, and assault with a deadly weapon. Trauma, with approximately 170,000 deaths per year and more than 400 deaths per day, is the 4th leading cause of death for all ages. Trauma kills more Americans than stroke and AIDS combined, and it is a leading cause of disability for survivors according to the CDC.
A trauma center is a hospital equipped and staffed to provide emergency medical services to patients who have sustained a traumatic injury. Although an emergency room also treats ill and injured patients, a trauma center is designed to treat severe, life-threatening injuries, including blunt force and penetrating trauma. Each trauma center is part of a larger system that uses state and local resources— hospitals and specialized equipment, physicians, surgeons, healthcare staff, ambulances, helicopters, paramedics, and emergency management teams—to achieve the best possible outcomes for patients. Trauma centers grew out of the realization that traumatic injury requires experienced physicians and surgeons who specialize in multidisciplinary treatments and specialized resources available 24 hours a day.
The concept of a trauma center was developed in Baltimore at the University of Maryland during the 1950s and 1960s by thoracic surgeon and shock researcher, R Adams Cowley, MD. The R Adams Cowley Shock Trauma Center was the first shock trauma center in the world. Trauma center levels across the United States are identified in 2 fashions—a designation process and a verification process. Trauma center designation is a process outlined and developed at the state level; for example, Georgia has 5 levels, while Florida has 2 levels. Trauma center verification is an evaluation process completed by the American College of Surgeons (ACS) to evaluate and improve trauma care.
The categories that define national standards for trauma care hospitals and the specific levels (i.e. Level I, II, III, IV, or V in the state of Georgia) refer to the types of resources available in the trauma center, including speciality physicians, hospital staff and equipment, participation in trauma research, healthcare professional education and injury prevention, and the number of patients admitted annually. Special trauma centers, such as pediatric and burn centers can be part of a larger trauma center or a separate facility. The majority of low-level trauma patients can be appropriately cared for at lower-level trauma centers. Patients with injuries that threaten life or limb can be transported to a level I or level II facility within the local geographic area.
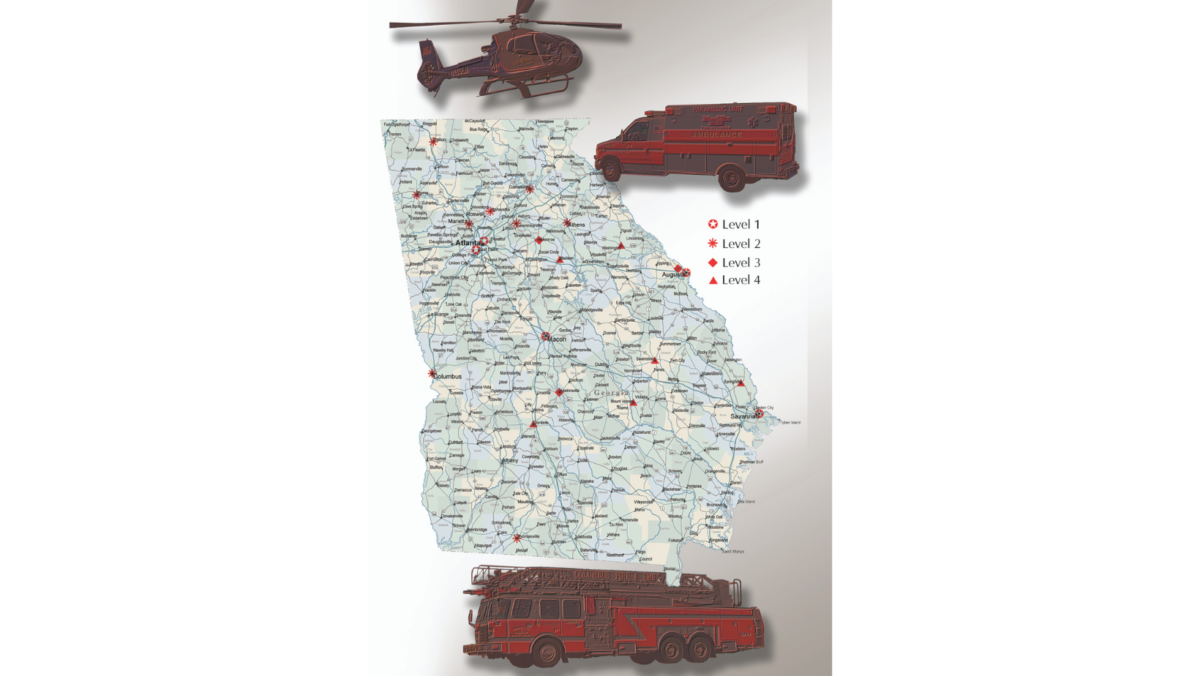
The Georgia Trauma Care Network Commission was established on May 11, 2007, to create a trauma system for the state of Georgia and to act as the accountability mechanism for distribution of trauma resources appropriated each fiscal year by the legislature. Funding the cost of a trauma center can be challenging for the various facilities and state legislatures. The Georgia Department of Human Resources designates the assigned trauma center level classification. Currently in Georgia, there are 20 trauma centers that are active at levels I thru IV of trauma designation.
When a hospital is designated as a trauma-care facility, the hospital must be prepared for any individual with a traumatic injury who comes through the door. Often, trauma teams are in a race against time. The first hour after an injury occurs, the so-called golden hour, can mean the difference between life and death. Rapid access to trauma care is often the patient’s best hope for a good outcome.
Trauma center levels in Georgia
The levels that classify a trauma center are based upon the care provided, staff qualifications, and the amount and type of equipment available.
Level I
A level I trauma center is a comprehensive regional resource that is a tertiary (high level, speciality care) referral facility essential to the trauma system. A level I trauma center is capable of providing total care for every aspect of injury, from prevention through rehabilitation.
Elements of a level I trauma center:
- Provides 24-hour in-house coverage by general surgeons, a full range of specialists, and specialty care resources, such as orthopedic surgery, neurosurgery, anesthesiology, laboratory services, emergency medicine, radiology, internal medicine, plastic surgery, oral and maxillofacial, pediatric, and critical care.
- Serves communities in nearby regions.
- Provides leadership in prevention and public education to surrounding communities.
- Provides continuing education programs for the trauma team members.
- Incorporates a comprehensive quality assessment program.
- Operates an organized teaching and research program to help direct new elevations in trauma care.
- Operates a program for sepsis, or substance abuse screening and patient intervention.
- Meets the minimal requirement for annual volume of severely injured patients.
Level II
A level II trauma center can initiate definitive care for all injured patients, but may need to transfer some patients to a level 1 center.
Elements of level II trauma centers:
- Provides 24-hour immediate coverage by general surgeons, and speciality care coverage, such as orthopedic surgery, neurosurgery, anesthesiology, emergency medicine, radiology, and critical care.
- May refer tertiary (high level, specialty care) needs, such as cardiac surgery, hemodialysis, and microvascular surgery to a level I trauma center.
- Provides trauma prevention and continuing education programs for staff.
- Incorporates a comprehensive quality assessment program.
Level III
A level III trauma center provides assessment, surgery, intensive care, and stabilization of injured patients in emergency operations.
Elements of a Level III trauma center:
- Provides 24-hour immediate coverage by emergency medicine physicians and prompt availability of general surgeons and anesthesiologist.
- Incorporates a comprehensive quality assessment program.
- Transfers patients requiring more comprehensive care to a level I or level II trauma center.
- Provides backup care for referral and community hospitals.
- Offers education of the nursing and allied healthcare professional or the trauma team.
- Involved with prevention efforts and an active outreach program for its referring communities.
Level IV
A level IV trauma center provides advance trauma life support before transferring the patient to a high-level trauma center. The center provides evaluation, stabilization, and diagnostic testing for injured patients.
Elements of a level IV trauma center:
- Provides basic emergency department facilities to implement Advanced Trauma Life Support (ATLS) protocol and 24-hour laboratory coverage. The trauma nurses and physicians are available upon the patient’s arrival.
- Can provide surgery and critical care services.
- Transfers patients requiring more comprehensive care to a level I or a level II trauma center.
- Incorporates a comprehensive quality assessment program.
- Involved with prevention efforts and an active outreach program for its referring communities.
Level V
A level V trauma center provides initial evaluation, stabilization, and diagnostic testing, and prepares patients for transfer to higher levels of care.
Elements of a level V trauma center:
- Basic emergency department facilities to implement ATLS protocols.
- Trauma nurses and physicians are available upon patient arrival.
- After hours activation protocols at the facility, but not available 24 hours a day.
- Can provide surgery and critical care services, if available.
- Transfers patients requiring more comprehensive care to a level I, II, or III trauma center.
Author: Robert M. Harris, MD | Columbus, Georgia
Further Reading: American Trauma Society, www.amtrauma.org
Last edited on November 29, 2023